Childhood experiences can affect our mental and physical health, but they don’t have to.
Jennifer Kelloff, MD, Permanente pediatrician, helps patients understand and learn from their experiences, so they can lead healthier lives.
- Before your 18th birthday, was a household member depressed or mentally ill or did a household member attempt suicide?
- Before your 18th birthday, was a biological parent ever lost to you through divorce, abandonment, or another reason?
- Before your 18th birthday, did you live with anyone who was a problem drinker or alcoholic, or who used street drugs?
These are three of 10 questions on the Adverse Childhood Experience (ACE) Questionnaire, which arose from a revolutionary mid-1990s study conducted in Southern California by the Centers for Disease Control and Prevention (CDC) and Kaiser Permanente. The study used a survey designed to measure the amount of abuse, neglect, and other negative experiences people faced in childhood. Why were two health organizations asking about childhood trauma? Because, as they discovered, children with high ACE counts are at increased risk for developmental delays, drug use, school issues, asthma, depression, anxiety and more. Childhood trauma has even been linked to a higher rate of heart disease, obesity, depression, and diabetes in adults.
That basic premise—our environment and our experiences impact our physical and mental health over the long term—guides the work of Permanente Pediatrician Jennifer Kelloff, MD. During her pediatric training, Dr. Kelloff recognized child abuse as a serious health problem and committed herself to becoming a leader in this field. As she became aware of the connection between various forms of violence, she partnered with adult medicine physicians to create a family violence prevention program. She is currently the medical director of Child Abuse Pediatrics and Prevention at Kaiser Permanente Colorado.
“All violence is interconnected,” says Dr. Kelloff, who was named to 5280’s 2018 Top Doctors list. “Boys who witness it are more likely to become abusers as adults. Girls who witness it are more likely to stay in abusive relationships as adults. Children are more likely to become bullies, commit suicide, or become victims of sexual violence. So, prevention in one area can lead to prevention in other areas.”
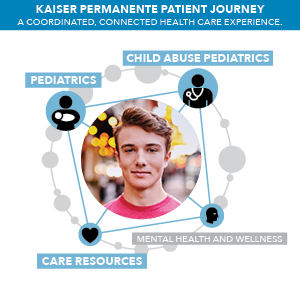
Although Dr. Kelloff works with child abuse victims and their care teams within Kaiser Permanente Colorado, the Colorado native also focuses on less severe cases, applying Trauma-informed Care model (TIC) practices with every patient to improve outcomes for all her patients. The TIC approach is founded on a shift in thinking: Instead of asking “What is wrong with you?” the TIC approach asks, “What has happened to you?”
Using this approach, Dr. Kelloff helps with even the everyday things parents might endure that can have subtle effects on the parent-child experience — the stress that comes with an extremely hectic schedule or the effects of a parent who is depressed. Dr. Kelloff might discover, for instance, that a mom who’s having trouble getting her baby to eat is so stressed at feeding time that it’s projecting onto her child, and that’s why he won’t eat. Maybe the mom’s reaction to stress is something she developed from her relationship with her own parents, but she has never thought about it before. Dr. Kelloff and her team help by offering tips to make meal time more relaxed.
“We know that your past experiences have a significant impact on how you react to things, how you are going to parent, what your health is going to be like. Trauma-informed care embodies the integrated, high-quality care we provide. It allows us to really understand how our patients’ experiences affect their health, and how they respond to treatment plans and recommendations and follow through,” Dr. Kelloff says.
“That’s also why we have made systemwide changes to screen for trauma and stressful life events in pediatrics, newly pregnant moms, and children with behavioral issues,” Dr. Kelloff says. “We are then able to listen to families, understand their needs and perspectives, and link them to the services that help them thrive.”
One example of this, Dr. Kelloff says, is connecting first-time mothers with Nurse Family Partnership, a program that helps parents and children realize their hopes and visions. “Here at Kaiser Permanente, we are engaging in efforts to strengthen the resilience and protective factors of children and families impacted by and vulnerable to trauma,” Dr. Kelloff says.
Adverse Childhood Experiences Are Common
ACEs cross all socioeconomic, racial, and ethnic boundaries. The original CDC study found that two-thirds of the 16,000 participants had experienced at least one ACE. Approximately 12 percent had experienced four or more, the tipping point at which serious health issues can emerge: An adult with four or more ACEs is 12.2 times as likely to attempt suicide, 7.4 times as likely to be an alcoholic, and 2.2 times as likely to have heart disease.
This information is vital to providing effective health care, which is why Dr. Kelloff and her team are working to disseminate this information—and the trauma-informed care model—throughout the Kaiser Permanente organization.
Take Jake*, a young boy who presented with uncontrollable asthma. His mom, Rachel*, brought him to Kaiser Permanente because nothing seemed to be helping her son. He’d maxed out his medications. He’d been checked for allergies. Rachel’s doctor, who had been trained in trauma-informed care, asked her if there were any consistencies in when Jake would have his asthma attacks. “It always happens when Dad comes home,” she responded. Upon further questioning, the doctor discovered that Rachel was experiencing domestic violence, and her son had witnessed Dad yelling and being physically aggressive. Kaiser Permanente connected Rachel with domestic violence resources, and once the situation was resolved, the boy’s asthma improved.
This is a prime example of why “holistic care is so important,” Dr. Kelloff says. “We can really affect the well-being of children—and children’s health outcomes when they become adults—by recognizing what more might be going on.”

Engaging with Dads
A focus on trauma-informed care isn’t just about the children, though. Pediatricians can also spot concerns with the parents during visits.
Maternal postpartum depression has received a lot of attention in recent years, which is a good thing. But fathers are getting left behind. “Rates of depression increase in the postpartum period for dads, as well,” Dr. Kelloff says. “We need to pay attention to them, too, because they’re critical in children’s development.” Studies have shown the rate of depression among adult males in the U.S. rises from 4.8 percent to 13 percent in the three to six months following birth. (In comparison, it increases from 8.5 percent to 10 to 20 percent for women.) Dr. Kelloff’s practice, in the Kaiser Permanente Westminster Medical Offices, completed a pilot study to screen and identify dads who are depressed and connect them to resources as well as engage them in conversations about their child’s health and support them in their parenting role.
Treating depressed fathers not only benefits them, but it also creates a healthier environment for the entire family. In fact, the number one protective factor against the potential consequences of trauma is safe, stable, nurturing relationships and environments. And, says Dr. Kelloff, it helps to know that no one is alone when it comes to having a hard time. Having a high number of ACEs, dealing with mental health issues, or just struggling to adapt with a new baby in the home is common. “Because Kaiser Permanente is an integrated system, we have lots of points where we can stop this cycle from progressing,” Dr. Kelloff says, adding, “It’s not all doom and gloom. Our adversities can make us stronger.”
*Names have been changed.
Dr. Kelloff is among more than 1,200 Permanente physicians serving Kaiser Permanente members across Colorado. Other Permanente physicians who were named to 5280’s 2018 Top Doctors list include:
Matthew S. Koehler, MD-Anesthesiology
Keri J. Propst, MD-Anesthesiology
Jennifer N. Kelloff, MD-Child Abuse Pediatrics
Laurent Lewkowiez, MD-Clinical Cardiac Electrophysiology
Elisa S. Kapler, MD-Dermatology
Barry A. Schoelch, DO-Diagnostic Radiology
Ryan Paterson, MD-Emergency Medicine
Deborah Fromm, MD-Family Medicine
Daniel P. Jones, MD-Family Medicine
Micheline Kuhr, MD-Family Medicine
Jennifer Osborne, MD-Geriatric Psychiatry
Margrit Juretzka, MD-Gynecologic Oncology
Alexander R. Menter, MD-Hematology, Medical Oncology
Frank Becky, MD-Internal Medicine
Lynn L. Rooney, MD-Internal Medicine
Stephen P. Johnson, MD-lnterventional Radiology
Morgan L. Swank, MD-Maternal & Fetal Medicine
Heidi Ray, MD-Neurology
Sirisha Komakula, MD-Neuroradiology
Eric K. Bode, MD-Nuclear Medicine
Jody L. Gibson, MD-Obstetrics & Gynecology
Tyler L. Skaife, MD-Orthopedic Sports Medicine
Timothy R. Muratore, MD-Orthopedic Surgery
Gary L. McDonald, MD-Otolaryngology
David Barclay, MD-Pediatric Anesthesiology
Brian Bagrosky, MD-Pediatric Radiology
Sorenna Kirkegaard, MD-Pediatrics
Sarah Beth Van Scoy, MD-Pediatrics
Edward T. Melkun, MD-Plastic Surgery
Kristy Bauman , MO-Pulmonary Disease
John Christopher Sohayda, MD-Radiation Oncology
John-Paul Morfin. MD-Rheumatology
Walter D. Conwell, MD-Sleep Medicine
David C. Gerhardt, MD-Sports Medicine
Christopher Jockel, MD-Surgery of the Hand
Justin Green, MD-Urology